

*A dilated pupil may be a sign of elevated intracranial pressure, secondary to herniation of the brain through the tentorium cerebelli, causing compression of the parasympathetic fibres within the oculomotor nerve (CN III), and is a neurosurgical emergency ExposureĮxamine carefully for lacerations, evidence of facial fractures, or depressed skull fractures. Glucose is the primary energy source used in aerobic metabolism for the brain and this demand can often increase depending on the severity of the head injury. Measure the blood glucose level and avoid hypoglycaemia.
FOREHEAD SKULL FRACTURE FULL
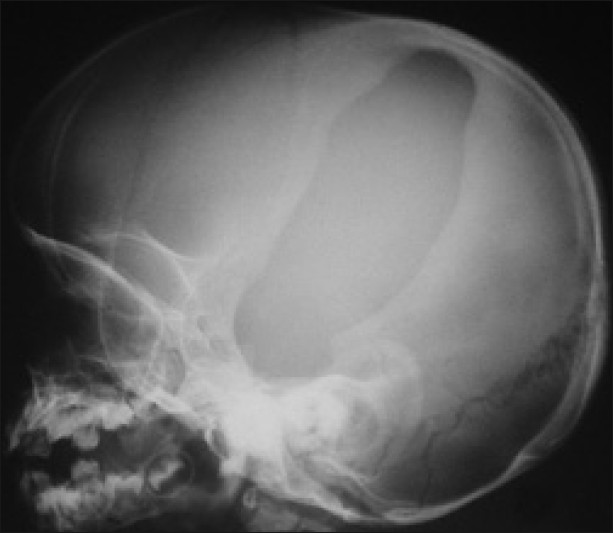
If the patient is conscious, assess for focal neurological deficit with a full neurological examination (both peripheral neurological and cranial nerve examination) The patient’s pupils must also be assessed regularly, both the size of the pupils and response to light*. This will typically be repeated every 30-60 minutes and repeated immediately if any evidence that the previous score has changed. In all patients presenting with a head injury, an accurate Glasgow Coma Scale must be recorded on admission. Ensure a good circulating volume is maintained from resuscitation with appropriate fluids Disability & Neurological examination BreathingĪfter the initial insult to the brain from the head injury itself the brain may become further damaged through secondary insult, most commonly and significantly is brain ischaemia secondary to tissue hypoxia.įor this reason, ensuring adequate ventilation (with a secure airway) and oxygenation is particularly important following head injury, limiting further brain damage from hypoxia CirculationĪside from securing the airway and maintaining oxygenation ensure adequate tissue perfusion to prevent any further secondary ischaemic damage to the brain. In those with a suspected cervical spine injury, a jaw thrust is typically the most appropriate, however can also be difficult if a collar is in place.īe wary in using airway adjuncts if there is extensive facial trauma, especially use of nasopharyngeal airways if there is any suspicion of basal skull fracture. If the GCS is 8 or less, or is rapidly deteriorating, then call the on-call anaesthetic team immediately to assist with airway management. *The decision whether to immobilise is usually made at the start of the initial assessment as it will affect subsequent airway manoeuvres and moving of the patient AirwayĪny patient with a GCS of 8 or less is at risk of being unable to maintain their own airway. In a patient suffering with head injury, always consider if the cervical spine may have also been injured certain mechanisms of injury often are accompanied together, particularly high energy trauma.Īt the start of the assessment* consider whether the cervical spine requires immobilisation via a semi-rigid collar, blocks, and tape (this may already be in place if the patient was brought in by ambulance) Head injuries can also be described by any resulting pathology that is associated with the head injury, such as superficial lacerationsor bruising, fractures (including linear, depressed, facial, basal skull fractures), haemorrhage outside the brain tissue (extradural/subdural/subarachnoid haemorrhage), haemorrhage within brain tissue (contusion/intra-cerebral haemorrhage), or diffuse axonal injury (DAI).įrank Gaillard, CC BY-SA 3.0, via Wikimedia Commonsįigure 1 – CT imaging showing a fracture-dislocation at C6/7 Table 1 – Classification of Head Injury based on Glasgow Coma Scale Head injury is classified as minimal, mild, moderate, or severe based on the patient’s Glasgow Coma Scale (GCS) mild head injury/TBI is also known as concussion.
FOREHEAD SKULL FRACTURE HOW TO
*The following document provides guidance on how to assess head injury in adult patients Classification The clinical outcomes from head injury can be significant it is currently the leading cause of death and disability in adolescents and young adults, hence a thorough and accurate clinical assessment of head injury at an early stage is imperative*. Head injury is one of the most common presentations to emergency departments worldwide, accounting for 1.4 million A&E attendances in the UK alone every year.


 0 kommentar(er)
0 kommentar(er)
